Delegates updated on HPAI response

Delegates updated on HPAI response
Story and photo by R. Scott Nolen
The AVMA House of Delegates (HOD) on June 20 heard from colleagues representing agencies and organizations responding to a multistate outbreak of highly pathogenic avian influenza (HPAI), specifically avian influenza virus type A (H5N1).
Speakers from the HOD’s House Advisory Panel and constituent allied veterinary organizations covered the current state of affairs and the challenges veterinarians in the poultry and dairy industries are facing, as well the efforts being taken to protect public and animal health.
Dr. Katherine Weathers, a poultry veterinarian with more than two decades of experience dealing with avian influenza and delegate for the American Association of Avian Pathologists (AAAP) in the HOD, told the House what they can expect when it comes to these highly pathogenic viruses. “Avian influenza is not going away.”

The AAAP has developed specific tools to help producers deal with an HPAI outbreak. “AAAP members are responsible for the health and welfare of millions, if not billions, of poultry in this country and worldwide,” Dr. Weathers said, adding that the association has helped developed surveillance and biosecurity programs used by all the U.S. primary breeder flock producers, and for most of the commercial poultry produced nationally.
“So, when we're talking about cattle and poultry active surveillance, poultry has already set the stage for what’s happening,” she said.
The U.S. poultry industry is in its third year of a multistate outbreak of H5N1 viruses that have spilled over into roughly 200 mammal species. In March, the virus was identified for the first time in a herd of dairy cows in Texas. As of June 21, H5N1 infections had been confirmed in at least 112 dairy cattle herds in a dozen states: 25 each in Idaho and Michigan, 20 in Texas, 12 in Colorado, eight in New Mexico, seven in Iowa, six in Minnesota, five in South Dakota, four in Kansas, and one each in North Carolina, Ohio, and Wyoming.
Dr. Sarah Tomlinson, representative for the U.S. Department of Agriculture (USDA) Animal and Plant Health Inspection Service (APHIS) on the House Advisory Panel, opened the Thursday morning informational session, explaining that USDA scientists have determined through genetic analysis that a wild bird infected with H5N1 clade 2.3.4.4b, genotype B3.13 is most likely responsible for the spillover event involving cattle.
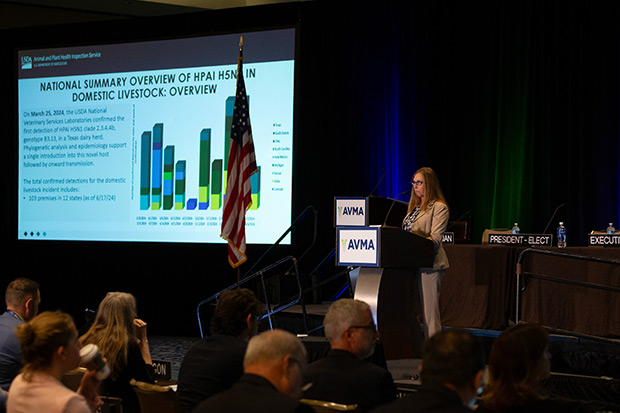
“Over the last only 90 days, there has been a tremendous amount of work to learn about this emerging disease in cattle being conducted by producers and state and federal veterinarians,” she said.
“We have conducted and administered epidemiology questionnaires,” said Dr. Tomlinson, who is a senior leader for Science and Information Technology for Veterinary Services within USDA APHIS. “We have done some on-farm intensive sampling. We have conducted wildlife and mature domestic species sampling on and around effected dairies, and we have now deployed three epidemiological strike teams.”
Recent laboratory pathogenesis studies indicate lactating cows are by far the largest and most affected vector for this disease, she continued. “This continues to be a form of morbidity in dairy cattle with mortality rates, including culling, 2% or less on average,” she said.
The disease is unpredictable, as it has shown up in asymptomatic dairy cattle, as well as those that show a high number of clinical signs over an extended period of time. Transmission appears to be multifactorial. APHIS has found that over half of affected premises are sharing equipment, such as trucks and trailers, and that three-quarters of affected premises have visitors who have frequent contact with the cattle.
The H5N1 virus also appears to have some ability to infect humans. Three individuals exposed to infected cattle have been confirmed as infected, according to Dr. Casey Barton Behravesh, the Centers for Disease Control and Prevention (CDC) representative on the House Advisory Panel.
Dr. Behravesh, director of CDC’s One Health Office, explained that conjunctivitis was the common clinical indication in all three cases, while the third affected individual also showed signs of respiratory illness. “Thankfully, there’s been no human-to-human spread detected to date, but that's something we continue to watch closely for and want to stay ahead of the curve on,” she said.
The CDC is conducting genetic sequencing of the virus from all human cases, and doing comparative analyses between human and animal sequences to assess the viruses for genetic changes that could indicate if the virus is adapting and spreading more easily, she continued.
“Today, there have been no changes detected that indicate the virus is more likely to transmit better from animals to people or from person-to-person,” Dr. Behravesh said. “And there's no indication that the virus would be resistant to antivirals or effective vaccines or diagnostics at this time.”
Concerning the safety of U.S. food supply, Dr. Thomas Vermeersch said, “The USDA is confident that the meat supply is safe, and part of that confidence is due to the fact that we have a rigorous meat inspection process associated with the release of meat for commerce.”
Dr. Vermeersh is the policy development division staff officer for USDA’s Food Safety and Inspection Service (FSIS), which he represents on the House Advisory Panel. He recounted how the USDA initiated three separate beef safety studies concerning avian influenza and meat from dairy cattle.
One study using samples from ground beef obtained from retail outlets in the states in which dairy cattle herds tested positive for H5N1 influenza virus found no viral particles to be present in the beef.
Two additional studies provided further evidence of a safe U.S. meat supply, according to Dr. Vermeesh.
Dr. Tristan Colonius of the FDA’s Center for Veterinary Medicine said research indicates that the commercial pasteurized dairy supply is also safe. “The good news is that the data is stacking up and (pasteurization) continues to work well against this virus,” said Dr. Colonius.
The FDA is working closely with its partners to understand and fill data and research gaps concerning the virus. For example, the agency is working with the USDA to test samples of pooled raw milk to characterize potential H5N1 levels and replicating commercial conditions of grade A milk production to further validate pasteurization.
Additionally, the FDA intends to support additional One Health research on interventions to prevent, control, or eliminate H5N1, with results becoming available soon, he said.