What Bird Flu Reminds Us About Influenza Pandemics
What Bird Flu Reminds Us About Influenza Pandemics
by Amesh Adalja
It is inevitable that there will be a next influenza pandemic in humanity's future. When it will occur and the identity of the culprit influenza strain are not fully answerable questions. There are myriad different avian influenza viruses constantly circulating, mutating, and regrouping in their natural waterfowl hosts.
As such, the prolific spread of the H5N1 influenza A virus in multiple avian species across the globe -- with spill into multiple mammalian species and a handful of human cases -- has prompted many to question whether an influenza pandemic caused by this virus is imminent. This is an important question that must be asked of all novel influenza viruses. However, the answers, when it comes to influenza, are not that simple and require placing this strain into a larger context of avian influenza more generally.
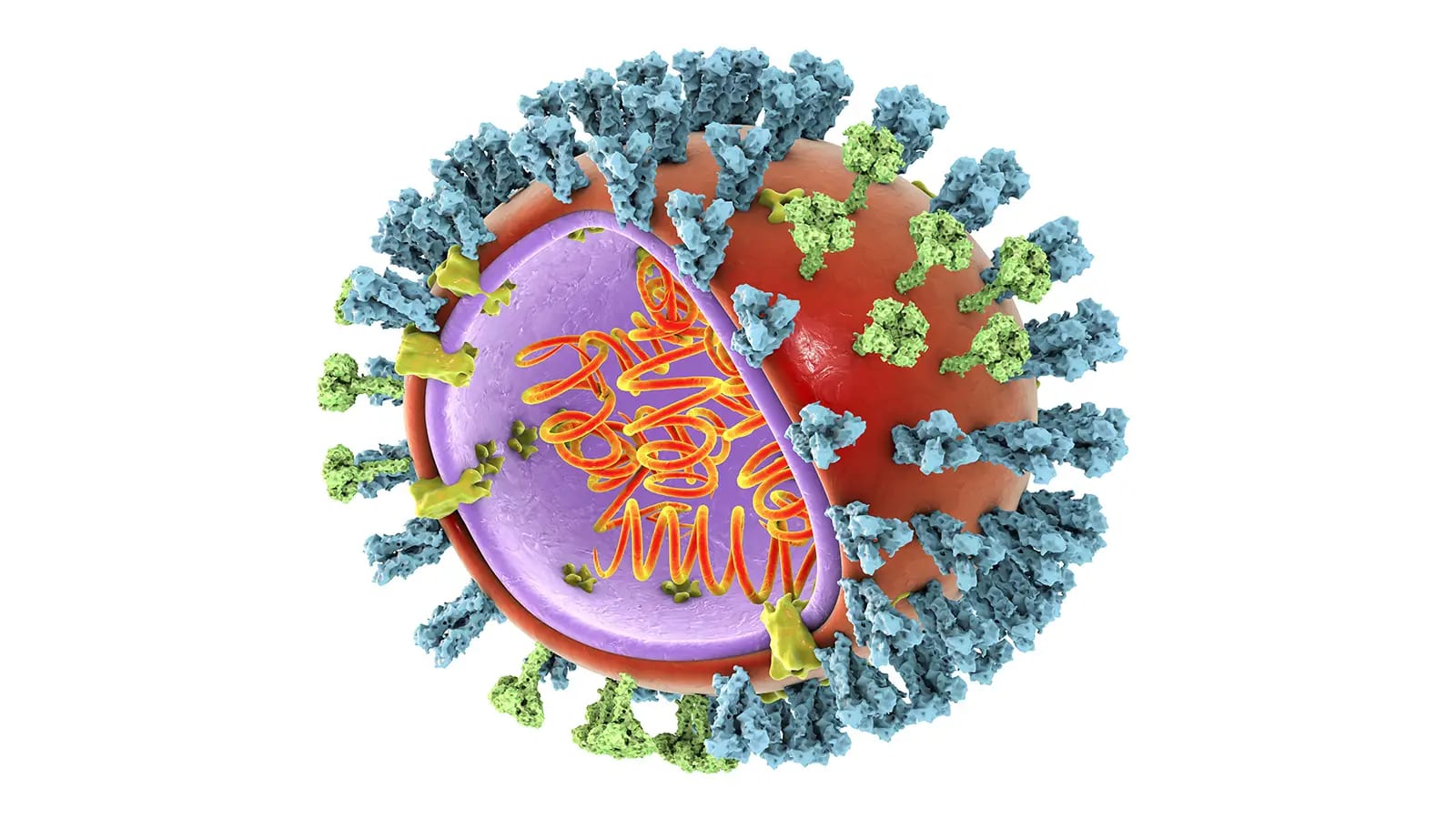
There are multiple steps necessary for an avian influenza virus to cause a human influenza pandemic. The first step -- capacity to infect humans -- is not easily traversed as most avian influenza viruses are incapable of infecting humans. The virus must find the human host hospitable in order to productively infect it.
Humans and birds are distinct enough that most of the viruses that infect birds cannot infect humans. Of the numerous combinations of the 18 hemagglutinin (H) varieties and 11 (N) varieties that naturally circulate in birds, only a select group have been able to even infect humans. Additionally, even if an avian origin virus is capable of infecting the human, the human may just be a dead-end host who will not spread it any further. Indeed, this is what mostly happens: a rare human with close contact to avian species (such as a poultry farmer) may get infected but no further human cases occur. Although the severity of the infection may range from extremely mild to extremely severe, no human-to-human spread occurs.
Despite this being the usual course of events, the feared scenario is an avian virus possessing or evolving the requisite genetics to be able to productively infect a human and be able to go on and infect another human. Sustained human-to-human transmission is the harbinger of an influenza pandemic and, in 1918, this sequence of events catapulted a wholly avian-origin influenza virus into a devastating global pandemic.
Is H5N1 destined to follow the 1918 H1N1?
The Story of H5N1 Influenza Viruses
First identified in birds in China in 1996, H5N1 did not reveal its full threat potential until six fatal human cases occurred in a 1997 outbreak in Hong Kong. These cases prompted aggressive culling in the live poultry markets to extinguish the risk. The virus, nonetheless, did not disappear -- it continued to circulate in its wild avian reservoir -- and reappeared to cause human infections again in 2003. This second appearance led to extensive pandemic influenza planning in the U.S., including stockpiling of vaccines and antivirals. To date, over 800 humans have been infected with H5N1 with about half succumbing to infection.
The Clades of H5N1
An important aspect of characterizing the H5N1 threat is understanding that this strain of influenza A is not monolithic but composed of multiple different clades, or subtypes, which are in turn composed of sub-clades. The original human infections were caused by clade 0 of a high-pathogenicity avian influenza (HPAI) Asian lineage H5N1 influenza A virus. Human infections that have subsequently occurred have been with various clades and sub-clades. Each clade and sub-clade has different proclivities for infection, severity, and antiviral susceptibility. As such, not all H5N1 viruses have the same pandemic or severe human disease potential.
The H5N1 in headlines today is clade 2.3.4.4b. This clade is distinct from other H5N1 clades that have caused severe human infections in the past. This important fact, often missing from reporting, is crucial to consider when trying to gauge the threat that exists from this virus today.
Human and Other Mammalian Infections With 2.3.4.4b H5N1
Thus far in this outbreak there have been about a half dozen human cases of H5N1. Most of these cases have been mild (the exception is one case in Ecuador of an H5, unknown N was severe), which may be an indication that this version of H5N1 is a significant departure from the more dangerous strains of H5N1. More significant is that there has been a striking rarity of infections (despite widespread exposure) compared to prior H5N1 outbreaks -- involving different clades -- where human cases were greater in numbers and more severe.
In contrast to the lack of human infections, the virus has been responsible for cases in multiple other mammalian species ranging from bears to seals to minks. The latter, because of its close similarity to ferrets (the human influenza surrogate) has raised concerns about mammalian adaption, especially given a specific mutation in one of the genes (T271A in PB2). It remains unclear, however, whether mammals are able to spread the virus amongst each other or infection is occurring due to consumption of infected birds. Regardless, any mammalian infection potential must be taken seriously especially given the number of different mammals involved, each giving the virus more opportunity to further adapt.
Other Avian Influenza Viruses of Concern
While there is currently a lot of justified focus on H5N1, it is important to recognize that other avian influenza viruses have been and are infecting humans as well. Some of these strains are quite alarming. One such virus is H7N9. This strain has been responsible for over 1,500 human cases occurring in six epidemic waves in China. Nearly 40% of those infected with H7N9 died. H5N6 is another avian influenza virus that merits close monitoring.
While each of these avian influenza viruses capable of infecting humans merit attention, determining which is most concerning is difficult. To help evaluate the relative risks of various avian influenza viruses on humans, the CDC developed an Influenza Rapid Assessment Tool (IRAT) that assesses the pandemic potential of avian influenza viruses using 10 attributes. Attributes include receptor specificity, human infection potential, disease severity, and other variables. Using this criteria, H7N9 is rated as a moderate to high risk virus with the most impact, whereas all H5N1s including 2.3.4.4.b are rated as moderate, with lower emergence and impact compared to H7N9.
Preparations
Irrespective of where any given virus falls on the IRAT ranking, if it has some significant risk of causing human disease, several important actions should be undertaken. These include: development of pre-pandemic vaccine stock that can be used for vaccine production if the need arises; stockpiling of vaccines for the highest risk viruses; testing of antiviral susceptibility of various strains; and vigilant surveillance of influenza viruses in humans, birds, and swine (which were the animal species that sparked the last influenza pandemic in 2009). All of these activities are currently being performed by the U.S. to some extent, but additional resources can enhance resiliency. Additionally, it is important to recognize that the threat of influenza is greatly enhanced by the lack of a universal flu vaccine that is broadly protective against various strains of the virus. To truly take influenza off the table as a threat, a universal vaccine will be required.
Regardless of the ultimate trajectory of the H5N1 strain currently engulfing avian species globally, it serves as a reminder of the absolute necessity to be proactive in the face of an unavoidable future influenza pandemic.
 The Mechanics of Infection with Avian Influenza Viruses
The Mechanics of Infection with Avian Influenza Viruses